Implantation failure is diagnosed when, after at least three cycles of in vitro fertilization or the transfer of more than ten good-quality embryos, pregnancy is not achieved.
Today we have highly effective solutions for every cause of implantation failure: blastocyst‐stage transfer (day 5), preimplantation genetic testing for aneuploidy (PGT-A) and assisted hatching.
What is implantation failure and why is it important to identify?
Embryo implantation requires a good-quality embryo, a receptive endometrium and effective communication between both. When pregnancy is not achieved after three IVF cycles or more than ten embryos transferred, it is called implantation failure. Early detection guides treatment and improves your chances of success.
Most common causes
- Embryonic: chromosomal abnormalities or difficulty hatching from the zona pellucida.
- Uterine: malformations, fibroids, adhesions, synechiae, endometritis or hydrosalpinx.
- Hormonal or metabolic: antiphospholipid syndrome, insulin resistance or obesity.
- Thrombophilias: clotting disorders.
How it is diagnosed
- Blood tests: hormones, metabolic profile, immunological markers and coagulation tests.
- Transvaginal ultrasound: identifies fibroids or malformations, measures endometrium (ideal ≥ 7 mm) and evaluates hydrosalpinx.
- Sperm DNA fragmentation: complements semen analysis if genetic damage is suspected.
- PGT-A: detects aneuploidies and selects euploid embryos.
- Zona pellucida monitoring: after culture to blastocyst to assess assisted hatching.

Reviewing your cycle history (oocyte yield, fertilization, embryo quality) helps personalize prognosis.
Treatment options
- Immunological: specific medication under medical supervision.
- Uterine: from hormonal therapies to minimally invasive procedures.
- Embryonic: cutting‐edge techniques:
Blastocyst transfer
Culturing embryos to day 5–6 allows selection of those with the highest implantation potential.
Preimplantation Genetic Testing (PGT-A)
By transferring only euploid embryos, you reduce the risk of failure and pregnancy loss, regardless of maternal age. This accelerates the path to pregnancy.
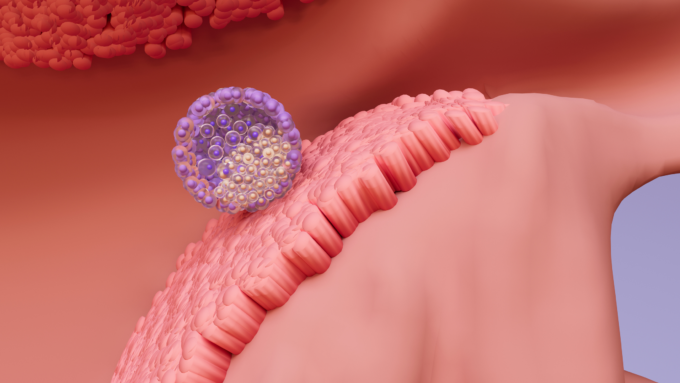
Assisted hatching
A laser creates a controlled opening in the zona pellucida to facilitate blastocyst–endometrium contact.
For more details, see Implantation Failures: Understanding the Challenge.
Frequently Asked Questions (FAQ)
How Does Maternal Age Affect It?
With age, oocyte quality declines and aneuploidy risk increases, making implantation harder. That’s why PGT-A is often recommended after age 35. But each case is unique: immunological, uterine and lifestyle factors also matter.
Why Does Endometrial Thickness Matter?
An endometrium ≥ 7 mm is associated with better receptivity. But vascularization and the implantation window also count. Specific tests help determine the ideal transfer timing.
Is Assisted Hatching Safe?
Yes, when performed by trained personnel using advanced laser. It takes seconds and, when done correctly, does not harm the embryo. It is recommended after previous failures and for blastocysts with thickened zona pellucida.
Why Shouldn’t I Self-Medicate?
Each hormone therapy or immunomodulator requires precise dosing and monitoring. Self-medication can create unnecessary risks.
Sources
- Practice Committee of the American Society for Reproductive Medicine. (2020). Evaluation and treatment of recurrent implantation failure: a committee opinion. Fertility and Sterility, 113(2), 278–285.
- MedlinePlus. (2023). IVF. https://medlineplus.gov/ivf.html
- American College of Obstetricians and Gynecologists. (2021). Assessment and treatment of recurrent pregnancy loss. ACOG Practice Bulletin, 225.
- ESHRE Recurrent Implantation Failure Working Group. (2019). Definitions and diagnosis of recurrent implantation failure: a consensus statement. Human Reproduction, 34(10), 215–226.
We know this journey can be challenging, but you are not alone. Every story is unique and deserves a tailored plan. If you suspect implantation failure, consult a reproductive specialist: together you will increase your chances of success.

